Education
Information is meant to empower us, not cripple us! Ask questions! Be proactive! You are your number one advocate!
What is Cancer?
Cancer is the uncontrollable growth of cells that destroys body tissue.
Why Early Detection?
5 Year Survival Rate Based off of Breast Cancer Diagnostic Stage, According to ACS
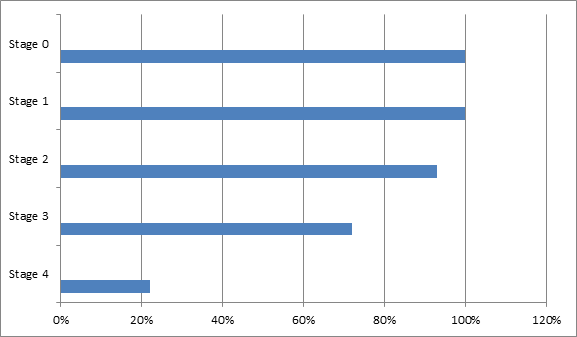
The data speaks for itself. Early diagnosis equates to a more favorable prognosis.
The American Cancer Society (ACS) states the 5 year survival rate after diagnosis for each breast cancer stage. The 5 year survival rate is the probability (based off of data collected from others with a similar diagnosis) of an individual living 5 years or more past their diagnosis. Please note, that these are estimates not absolutes. There are no guarantees; no one can predict with absolute certainty your longevity. Be sure to talk to your medical providers about your cancer, prognosis, and treatment plans. A cancer stage is determined based off of a series or requirements, including: size, location, lymph node involvement, and metastasis.
Stage 0 – (also called carcinoma in situ) refers to abnormal cells that haven’t broken free of their duct or lobule, depending on where it originated within the breast.
Stage 1– cancer is localized and small
Stage 2 and Stage 3 – cancer is larger, spread to nearby tissue or lymph nodes
Stage 4 – (also called metastatic breast cancer) cancer has spread to other parts of the body. Although there is no cure for metastatic, there are treatment options. Consult with your doctor.
Screenings & Early Detection:
So, we know early detection is critical. Now, what does that actually look like?
Breast Imaging w/ Radiologist, Dr. Sergio Dromi: Dr. Dromi (Director of Breast Imaging at Memorial) explains the different methods of breast imaging: mammograms, MRIs, and ultrasounds. He explains what mammograms are, how they work, and when women should begin their annual screenings. He covers breast density, screenings vs diagnostics, as well as 3D mammograms. Dr. Dromi also helps us better understand MRIs (including how they work), ultrasounds, biopsies, and more.
Self-breast exams
How Do You Do A Self-Breast Exam?
Hear what survivors urge women and young girls to know: Visit the Survivor link to hear their interviews.
“Know Your Own Geography!”
Christy – Survivor
Mammograms
Women who are 40 and over and are at average risk should talk to their doctors about having annual screening mammograms done. It’s recommended that women have the mammogram performed yearly as part of their regular health maintenance. A mammogram takes images of the woman’s breast; and it is used as a tool to screen for cancer. DenseBreast-Info explains the differences in the types of mammography.
Mammograms are also used to indicate your breast density. Many states now have breast density legislation, requiring you to be notified on your mammogram report of your breast density and how that affects your risk for acquiring breast cancer.
- Screening Mammograms – done annually after age of 40. They’re watching/screening to make sure their are no suspicious masses.
- Diagnostic Mammograms – done when you’ve noticed a mass or have another symptom warranting a ‘closer look.’
Ultrasounds
Ultrasounds use soundwaves to ‘investigate’ the breast tissue. The waves create an echo and bounce back off of masses, helping to create an image. Ultrasounds can be used to discern whether a discovered mass is solid or fluid filled. Fluid filled masses are cysts and are benign. Solid filled masses can either be fibroids (benign) or cancer (malignant). It’s possible that your provider may refer you for a biopsy if a solid mass is noted.
MRIs
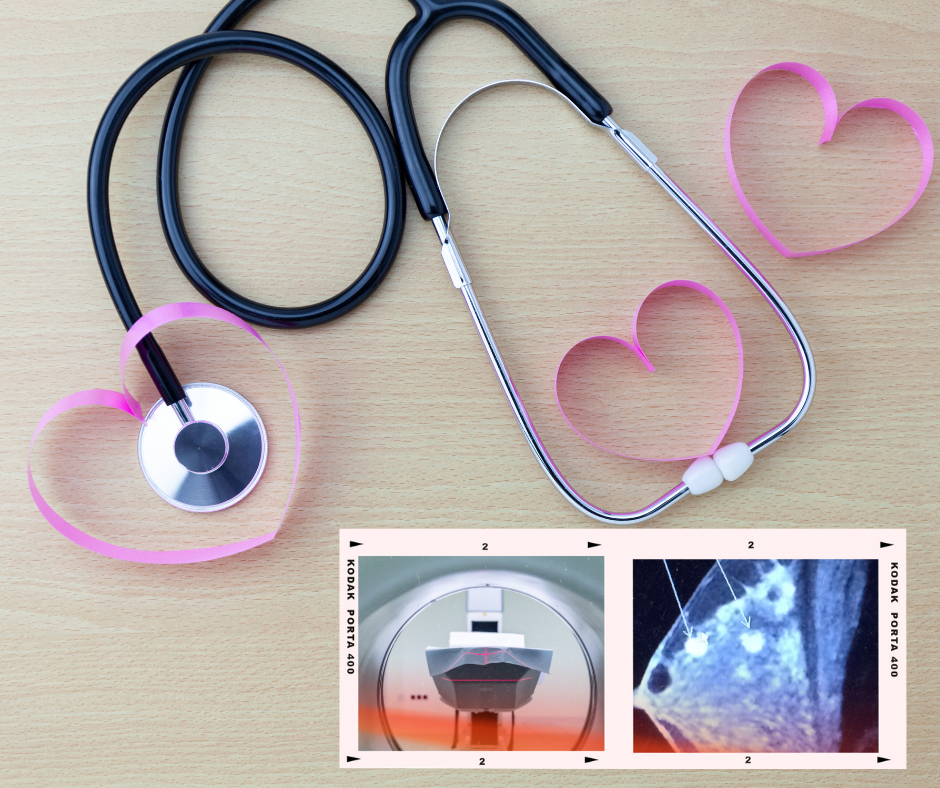
MRI stands for Magnetic Resonance Imaging. This is the test where you lie in a tube for 30-45 minutes while a machine makes a whole bunch of racket around you. MRIs are LOUD!
The human body is made up of lots of water; and since water has a polarity (Oxygen having a slightly negative charge, while Hydrogens having a slightly positive charge), MRIs are able to use proton charges, powerful magnets, and radio waves to create images.
Since cancer is vascular, they also administer a contrast material intravenously prior to the imaging to enhance the images.
MRIs are sensitive machines; and although they may be capable of seeing things that a mammogram can miss, they do create some “false-positives” because of their sensitivity. MRIs are also much more expensive.
Talk with your medical provider to review your personal medical necessity and risk factors to know whether an MRI is in your best interest.
What is breast density?

Learn more about Breast Density and Georgia Legislation at Margie’s Army Foundation
Hear from Margie Singleton in our podcast interview on breast density and Margie’s Law
Know your breast density! Not all breasts are created equal. Of course they come in different sizes and shapes, but density is a thing too (and that’s not something you can discern just from touching). Only a mammogram can tell you what your density is. Some breasts have dense tissue that makes it difficult to distinguish tissue from masses on mammogram screenings.
I was told that dense breasts look on imaging like you’re driving through a snowstorm with your windshield wipers on turbo, but you still can’t see anything. Talk to your doctors about your own breast density and what that means for you and your surveillance. Do you have dense breasts or not? What does that mean? How does it affect your risk?
Not only do dense breasts make it more difficult to see cancer on mammograms, but having dense breast tissue is also a risk factor.
Most states have dense breast legislation in place, requiring mammogram reports to include a description of your breast density on them. Margie’s Law went into effect July 1, 2019 in the state of GA. If you have dense breasts, your mammogram reports should read (in Georgia):
Your mammogram shows that your breast tissue is dense. Dense breast tissue is very common and is not abnormal. However, dense breast tissue can make it more difficult to detect cancer through a mammogram. Also, dense breast tissue may increase your risk for breast cancer. This information about the result of your mammogram is given to you to increase your awareness. Use this information to talk with your health care provider about whether other supplemental tests in addition to your mammogram may be appropriate for you, based on your individual risk. A report of your results was sent to your ordering physician. If you are self-referred, a report of your results was sent to you in addition to this summary.”
Breast Basics
The breast is made up of a series of ducts that connect lobules (milk producing glands) to the nipple. See diagram.
Hear from breast surgical oncologist, Dr. William Burak, Jr.
Dr. Burak explains the different kinds of breast cancer, the treatment options and their risk reduction, surgery expectations, and healing.
Breast Cancer Defined
I used to think that cancer was distinguished solely by where it was found. Breast cancer, I concluded, was therefore cancer found in the breast. This would imply that all breast cancers were created equal; however, that is not the case. There are several different kinds of breast cancer. Here’s a quick look at how they are distinguished.
1) Lobular vs Ductal
Cancer can originate in the lobules or the ducts.
- Lobules – are the milk producing glands
- Ducts – are the tunnels that connect lobules to the nipple.
2) In Situ vs. Invasive
Your breast is made of a series of ducts that link lobules. Cancer cells usually begin in one of those locations. If it stays contained in the duct for example, it is called in situ; whereas once it’s eaten a whole through those ducts and into regular breast tissue, it is called invasive.
Invasive ductal carcinoma is therefore cancer that originated in the ducts, but has broken free into the surrounding breast tissue. At that point, it can travel to the lymph nodes.
3) Tumor Grade
Based off of how ‘wonky-eyed’ those cancer cells look in comparison to normal breast tissue cells. It is assessed based on three criteria:
- Tubule Formation
- Nuclear Grade
- Mitotic Rate
The lower the grade (Grade 1) – slower growing, less likely to spread.
The higher the grade (Grade 3), the more aggressive the cancer. It’s faster growing and more likely to spread.
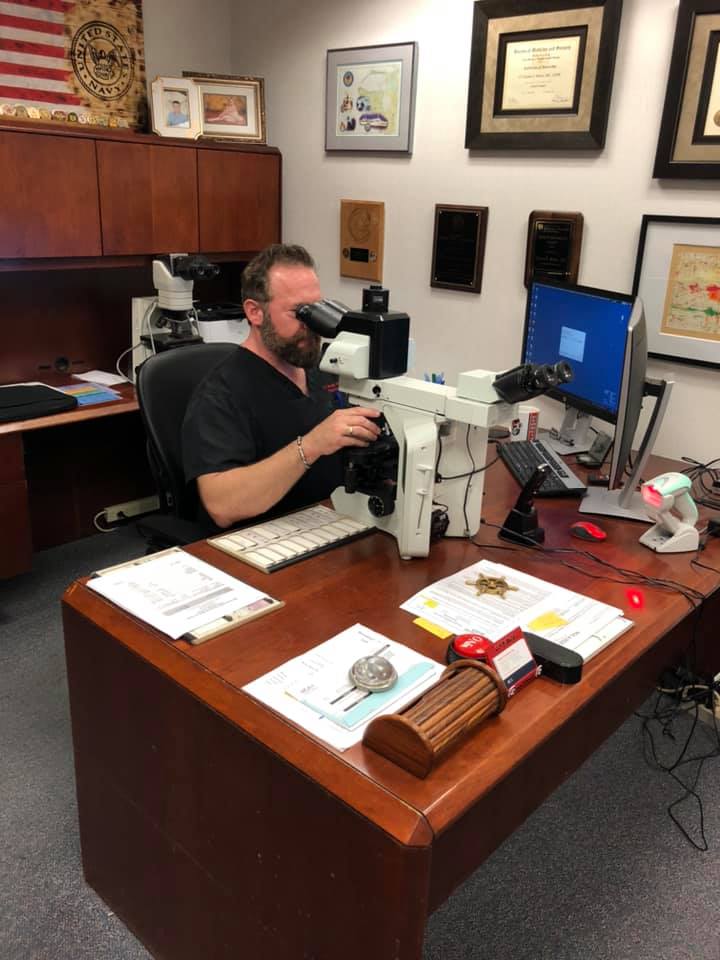
Pathologist examines slides 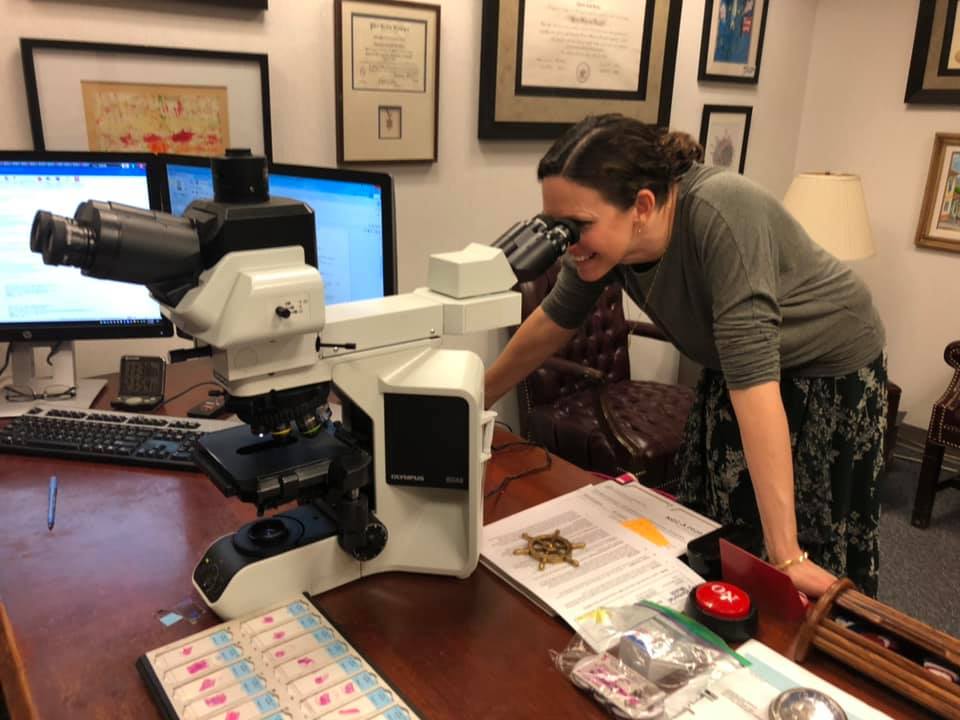
I get to take a peek at my cancer 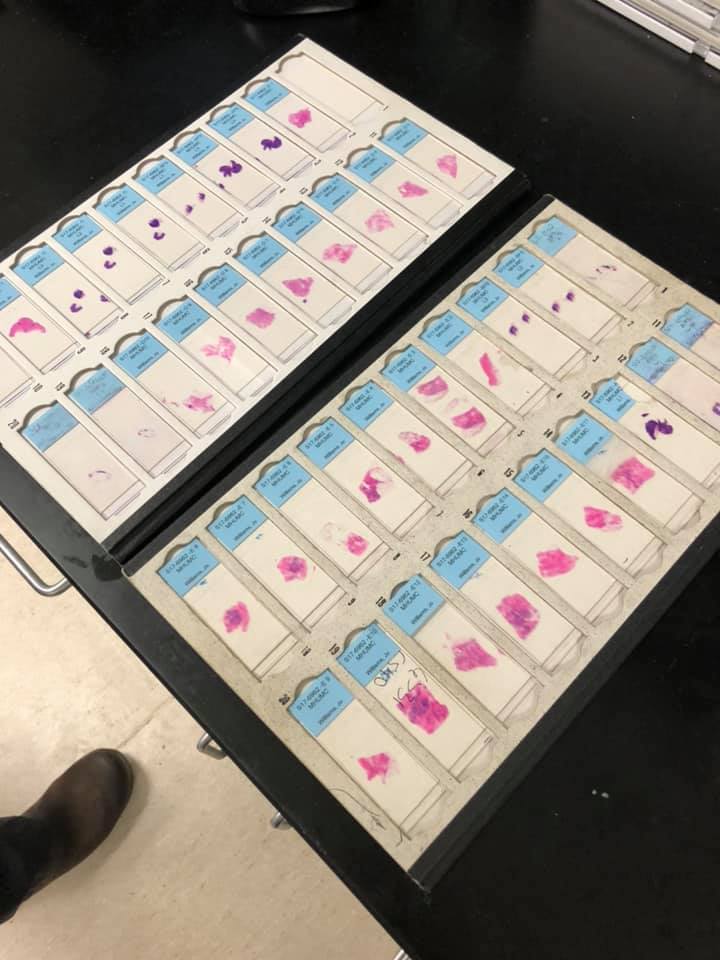
My cancer on slides
4) Hormone Receptors; HER2
When they biopsy your tumor, they will run tests that determine the presence of hormone receptors.
If someone is estrogen or progesterone positive – that means that their tumor cells have receptors that allow their cancer to grow within the presence of those hormones. You can think of it like food for the cancer. Estrogen/progesterone positive cancers like to eat (and grow) with those hormones. When you take those hormones away, then the cancer’s food source is cut off and the cancer is less likely to flourish. (Estrogen and progesterone negative would mean that the tumor doesn’t have those receptors…aka they don’t eat that food).
Consequently, estrogen and progesterone positive tumors can be treated with medicine that limits those hormones in the body. However, this hormone therapy would not prove beneficial for estrogen and progesterone negative cancers (because those tumors don’t feed off of that food).
HER2 – refers to the presence of a protein that the cancer makes.
Triple Negative: Means that a cancer is estrogen and progesterone negative (hormone therapy won’t work) AND HER2 negative. Therefore, triple negative breast cancer is typically more aggressive and harder to treat.
Triple Positive: Means that the cancer is estrogen and progesterone positive AND HER2 positive. Drugs that lesson the hormone presence AND those that target HER2 could be used
Estrogen and Progesterone positive/ HER2 negative: Means that the cancer is fed by those hormones and can thus be treated with hormone therapy; but it does not have HER2.

Examining the breast tissue 
Finding tumors 
Testing Hormone Receptors
Understanding Pathology with Pathologist, Dr. Charles Todd Bruker, MD.
The information pathologists gather provides our surgeons, oncologists, and radiation oncologists with critical information that’s used to determine the most appropriate treatment plans for our cancer. Pathologists help discover the tumor grade; estrogen, progesterone, and HER2 status; lymph node involvement, and more. Dr. Bruker gives us a tour of the inner workings of the pathology lab. Read what he has to say or listen to our podcast interview with him.
5) Stage 0-4
(stage is given based off a series of criteria: size, location, whether or not it has spread) See graph above.
Interesting point: If breast cancer makes it to the lymph nodes and travels (metastasizes) to say, your bones…. That is not referred to as bone cancer. Rather, it’s stage 4 metastatic BREAST CANCER. (The cancer originated in your breast but moved to a new location).
6) IBC — Inflammatory Breast Cancer
Not all breast cancer has a lump. IBC, although rare, is an aggressive breast cancer that essentially blocks the lymph system in the breast’s skin causing it to appear inflamed.
- 1 out of 3 diagnosed with IBC will have already metastasized
- For more information about IBC, read what the National Cancer Institute has to say.
Understanding Inflammatory Breast Cancer with Survivor Lindsey Wirht. What exactly is it? What are the signs and symptoms? How is it diagnosed? And what else do you need to know? Listen to her interview to understand it better.
Breast Surgeries
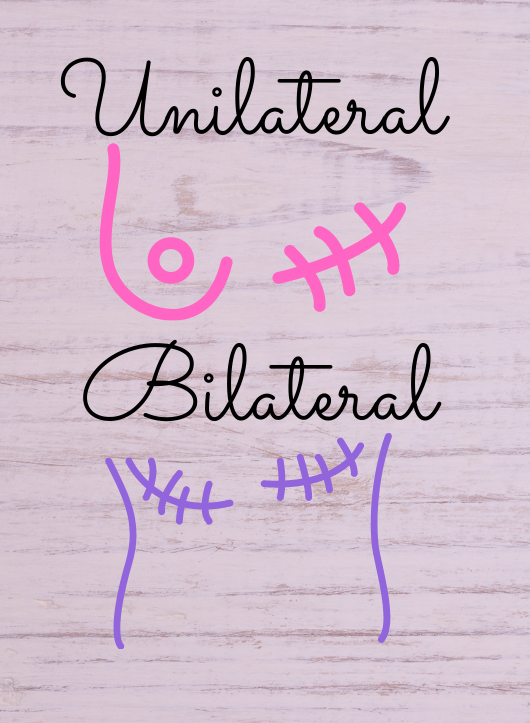
Lumpectomy – removal of part of the breast
Unilateral Mastectomy – removal of one breast
Bilateral Mastectomy – removal of both breasts
Plastic Surgery
After the removal of one or both breasts due to cancer, some women may opt to have reconstruction done. Most insurances will cover this, deeming it reconstructive rather than cosmetic surgery.
Still, there are several options:
- DIEP Flap – (from abdomen, buttocks, or back)
- Reconstruction with Implants
- Straight to implant during mastectomy
- Using expanders to first reconstruct the breast, followed by switch-out surgery for implant.
Hear what plastic surgeon, Dr. Carl Pearl and his nurse Mary say about reconstruction in our interview.
Chemotherapy

Chemotherapy is a systemic treatment. Drugs are given intravenously (either through an IV or a portacath), and they travel/treat throughout your entire body. Of course, discuss with your doctor the best treatment options for you as well as the potential risks and side effects.
Different chemotherapy drugs can be administered for breast cancer, though they’re typically given as a combination treatment (meaning you receive two of the chemo drugs during treatment).
Examples of common chemo drugs for breast cancer include:
Cytoxin
Taxotere
Adriamycin
Why a Combination Treatment?
Different chemotherapy drugs target cancer cells at different stages in their cellular division. So, by giving a combination treatment you maximize the number of cancer cells that are targeted.
When they’re administered?
- Neoadjuvant Chemotherapy – chemotherapy administered prior to surgery
- Adjuvant Chemotherapy – administered after surgical removal of cancer
Hear from a NP in medical oncology.
Vanessa Brink (NP in medical oncology) helps us better understand who can benefit from treatment, why combination treatments are typically given, what you can expect when you go in for transfusions, how hormone receptors and HER2 can affect your treatment, what potential side effects are, and why it’s important for you to talk with your doctor about any concerns. We also learn more about the oncotype test and how it can be used to predict the effectiveness of chemo on your specific tumor.
Radiation Oncology
Radiation therapy is a localized treatment, targeting specific areas.
- CT Scan & Mapping –
- Done prior to treatment
- CT scan is used by the radiation oncologist to make a personalized mapping for your treatment. (everybody’s lungs, hearts, etc, are in slightly different locations)
- Allows radiation oncologist to target the areas they want and avoid the areas that they don’t
- Bolus –
- Tissue equivalent
- Sometimes used to bring radiation dosage closer to the skin
- Ways to Ensure Exact Alignment
- Foam pillow, contoured to your body
- Blue tape and/or tattoos to aide in alighnment
- Xrays prior to administration
Hear From Radiation Oncologist, Dr. Michael Hasselle, M.D. to learn more about radiation therapy and what you can expect
Helpful to Know
- Machines have lots of working parts, and safeguards. It’s not unheard of for the machine to be down one day. If this happens, know that it’s normal; and the missed appointment will likely get tacked onto the end
- The machine circles around you; it NEVER TOUCHES YOU (This was huge for me after scalpels and needles from prior treatments).

door to radiation 
radiation machine 
skin reddening
Lymphedema
The Lymphatic System
- The lymphatic system works to clear up infections in the body.
- The lymph nodes make up part of this system.
- When lymph nodes are damaged (or removed during surgery), then our risk for developing the condition increases.
- Lymphedema involves the uncomfortable and incurable swelling caused by the damaged lymphatic system’s inability to function properly.
- No cure; but are risk reduction practices.
Risk Reduction Practices
The idea is to prevent nicks, or cuts and scrapes from the side of the body where lymph nodes were removed so that the lymphatic system in that area doesn’t get overworked, triggering lymphedema. The same logic is why women who’ve had lymph nodes removed under their arms during surgery should not have blood drawn or blood pressure taken on that arm.
Risk Reduction Practices
More on Lymphedema
Maintenance
Speak with a a lymphedema specialist. They are best trained to assist you with manual lymph drainage, compression bandaging, and exercises.
Hear from Lymphedema Expert, Corie Turley in Our KotF Interview
My Risk & Genetics
My Risk
Tyrer-Cuzick Risk Model
- Well studied, widely available software program for predicting one’s overall lifetime risk for acquiring breast cancer
- Considers data/risk factors such as:
- Family history
- Hereditary cancer mutations
- Personal risk factors
- Age/height/weight
- Age at first delivery
- Ashkenazi Jewish decent
- Hormone use
- Age at first period
- Number of full term babies
- Menopause
- Breast Density
- Lifestyle (alcohol, smoking, exercising)
- Generates a Score for Lifetime Risk
| <15% | 15-19% | >20% |
|---|---|---|
| Average Risk | Intermediate Risk | High Risk |
High Risk: >20% Lifetime Risk
American Cancer Society (ACS) recommends annual MRI and mammography regardless of density.
Hear from Jen Davis and the High Risk clinic at Memorial Hospital
Genetic Mutations (Hereditary)
Genetic testing can examine your genes and find out whether or not you’re at an increased risk for cancer. BRCA 1 and BRCA 2 (commonly referred to as the breast cancer mutations) can be detected in this manner. BRCA1 is found on chromosome 17 and BRCA2 is found on chromosome 13. These genetic mutations can be inherited from one’s mother or father. Although they are the most common hereditary mutations for breast cancer, they are not the only ones. Speaking with a genetic counselor can help determine your risk and prevention/treatment options.
Read More on Our Genetics Post
Hear From a Genetic Counselor
Hear More About Genetics
FORCE
Learn more about Clinical Research Trials, prevention, treatments, and quality of life studies for Hereditary Cancers by visiting FORCE’s Featured Studies Page.
Epigenetics
Genetics is the study of how traits get passed down from one generation to the next. Epigenetics, having the prefix epi (meaning ‘on top’), refers to how our DNA interacts with proteins and receives notifications of what genes are to be turned on and which are to be turned off.
Tumor suppressor genes- genes that tell old cells when they’ve reached the end of their life cycle and are to die off. If the old cells don’t get the message to die off, then they continue to replicate out of control. That is essentially cancer. So, tumor suppressor genes are good because they prevent those old cells from growing out of hand. Tumor suppressor genes therefore suppress tumor growth.
(Note: BRCA genes are tumor suppressor genes – you want those; its the MUTATION in the BRCA genes that causes problems).
Analogy: If your DNA is like the blueprint for your house, then epigenetics helps determine which lights in the house are on. (what genes are turned on or off inside individual cells).
Your DNA is the same inside each of your cells. Your skin cells, blood cells, neurons – they all have identical DNA — YOUR DNA. However, these cells look and function differently. Why? Because skin cells have skin cell genes turned on and liver ones turned off. Epigenetics is essentially the study of how certain genes get turned on/off. Remember, we don’t want those tumor suppressor genes to be turned off.
Previvors, Survivors, Thrivers
Patients may prefer one of these words over another, and that’s okay! However, for those who are unfamiliar with the terminology, here is a very generalized idea.
Survivor
- One who has dealt with a cancer diagnosis;
- One who is dealing with a diagnosis/treatments;
- One who has gone through treatment, and emerged on the other side of the battlefield with no evidence of disease.
Previvor
- Refers to those who don’t yet have cancer but have an extremely high risk for developing it (often noted by a genetic mutation, such as BRCA). A BRCA mutation can, for example, increase one’s lifetime susceptibility of developing breast cancer from the general population’s 7.3% risk to an 84% or 90% cancer risk!! THAT is significant. Previvors can choose to get out ahead of cancer by means of prophylactic surgeries. Prophylactic means: intended to prevent a disease. So, a prophylactic mastectomy would therefore mean a mastectomy done in order to reduce ones risk of developing breast cancer.
Listen to our Genetics Podcast to learn more about basic genetics and understanding BRCA mutations
Read more about the weighty choices to consider when dealing with a hereditary mutation such as BRCA.
Hear directly from a previvor in our interview with Stephanie. She talks about the mutation, the concerns, the surgery, and previving.
Thrivers
- A term that some women prefer to use in place of survivor. Sometimes women feel that if they haven’t reached the end of their treatments, they are unable to claim the mark of ‘survivorhood’. They may choose to identify themselves as a ‘thriver.’
- This term can be used by those who are currently in the midst of their storms
- Can also refer to someone who is dealing with a recurrence and/or living with stage 4 metastatic breast cancer.
Emotional
Emotional hurtles (and wounds) are just as real and part of this journey as the physical ones. YOU ARE NOT ALONE!! Anxiety, depression, and PTSD (Post-Traumatic Stress Disorder) are not uncommon. Breast cancer and the treatments themselves are life-altering…sometimes even traumatic. Give yourself permission to be human; and work towards healing these wounds too.
- Psychotherapy – or talk therapy, is a way for people to process through their emotions in a safe, nonjudgmental atmosphere with a licensed clinician
- Cognitive Behavioral Therapy (CBT): helps you recognize patterns of negative thinking that you may have so that you can then alter your behaviors for facing challenges in a healthier way.
- Eye Movement Desensitization and Reprocessing (EMDR) has been used to treat trauma and PTSD. It involves recalling the traumatic event while a therapist uses bilateral stimulation (ex: following a light or tapping) while readdressing your trauma. The idea is that it acts like the processing that we’re able to do in REM sleep, thus helping our memories better process our trauma.
- Dialectical Behavioral Therapy (DBT): founded by Marsha Linehan; includes the idea of Radical Acceptance.
Radical acceptance rests on letting go of the illusion of control and a willingness to notice and accept things as they are right now, without judging.
Marsha Linehan
Finding a Therapist
Learn more about therapy and opportunities available.
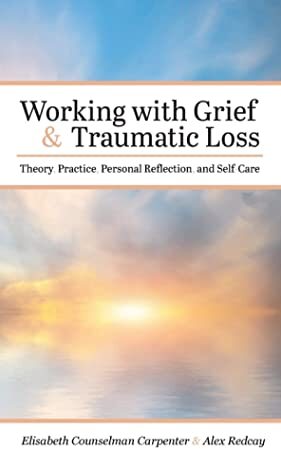
Grief & Traumatic Loss
A cancer diagnosis and the treatments that follow can be a traumatic experience. (We’re human.) Grief accompanies loss, and we’ve most definitely experienced “loss”.
For Example (just a few):
- Loss of Health
- Loss of Body Parts
- Loss of Sense of Safety in the World
- Loss of Sensation
Author, Educator, and Clinician: Dr. Elisabeth Counselman Carpenter, PhD, MSW, LCSW
Dr. Elisabeth Counselman Carpenter (Beth), co-author of ‘Working with Grief and Traumatic Loss’, explains what grief and traumatic loss are, how the theories on trauma and grief are applicable through this breast cancer lens, and what evidence-based strategies may be beneficial. She also explains what activities can be helpful for processing through the grief, what self-care looks like, and how it is beneficial. Traumatic experiences are transformative, and Beth helps us see ways to sift through the mess and rise again with a newer normal after breast cancer.
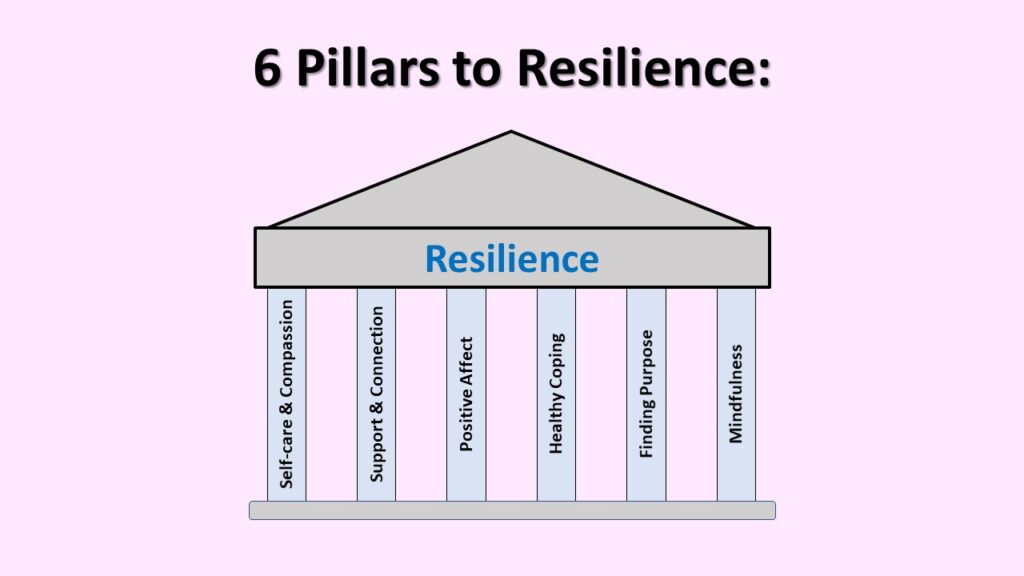
Learn More about Resilience
Our Free Resilience Course – consists of 10 short YouTube videos, where we explain how we can rewire our brains for resilience with six key pillars:
- Self-Care & Compassion
- Support & Connection
- Positive Affect
- Healthy Coping
- Finding Purpose
- Mindfulness
Hear from Other Survivors
Growing Medical Needs Requiring Public Attention
Change is made on a much larger scale when we can understand and address some of the disparities between medical needs and resources available. Education and accessibility to care are among the two biggest barriers. In our podcast interview on the matter, we explore them through pertinent topics such as:
- Understanding your risk
- Insurance coverages and concerns
- Biases and fears.
- The growing need for bridging the gap between physical and emotional (our medical and psychological) healing.
VOCABULARY
DCIS –(Ductal Carcinoma In Situ) – cancer that originated in the ducts and has NOT broken out into surrounding tissue….cancer is contained in its original spot.
Invasive ductal carcinoma – cancer that originated in the ducts and HAS broken free into surrounding tissue.
Lymph nodes– part of the body’s immune system. There are 100s throughout the body, connected by a series of vessels; and their job is to help filter and protect your body from harmful substances. However, if cancer cells reach the lymph nodes, it’s like they’ve made it to your body’s train station. Cancer can easily hitch a ride to another destination in your body: bones, liver, brain, etc. It terms of cancer, you do NOT want it to have reached the lymph nodes.
Lymphodema– a condition caused by the removal of lymph nodes; can cause swelling. Surgeon’s will often remove lymph nodes during surgery to ascertain whether or not cancer had made it there. It’s an important piece of information to acquire because it can help determine your stage of cancer, treatment plans, and prognosis. However, the more nodes you have removed, the higher your risk is for developing lymphedema. Read about Risk Reduction practices for lymphedema here.
Metastatic – cancer that has moved to another part of the body.
Neuropathy – loss of feeling/numbness/tingling in your hands or feet due to nerve damage. It’s a possible side-effect of chemotherapy.


